This story first appeared in the Tri-City News on March 15, 2024
A nondescript white panel van is delivering relief to homeless populations in the Tri-Cities, Burnaby, New Westminster and Maple Ridge.
Sometimes it even helps save a life.
During a recent visit to the 3030 Gordon shelter in Coquitlam, medical professionals from the Integrated Homelessness Action Response Team (IHART) mobilized when a man overdosed on the sidewalk.
As his worried street buddies gathered round and coaxed the man to wake up, registered and practical nurses administered naloxone and notified emergency services. After several tense moments he was responsive and sitting up. Minutes later he walked away, getting on with his day as if nothing unusual had occurred.
While the IHART program has been operating since 2022, it’s been bringing its suite of health care, mental health and outreach services to the streets in a van since January.
Lower barriers
The program’s co-ordinator, Paolo Palomar, said the idea is to lower barriers to obtaining health care for a population that would otherwise have none.
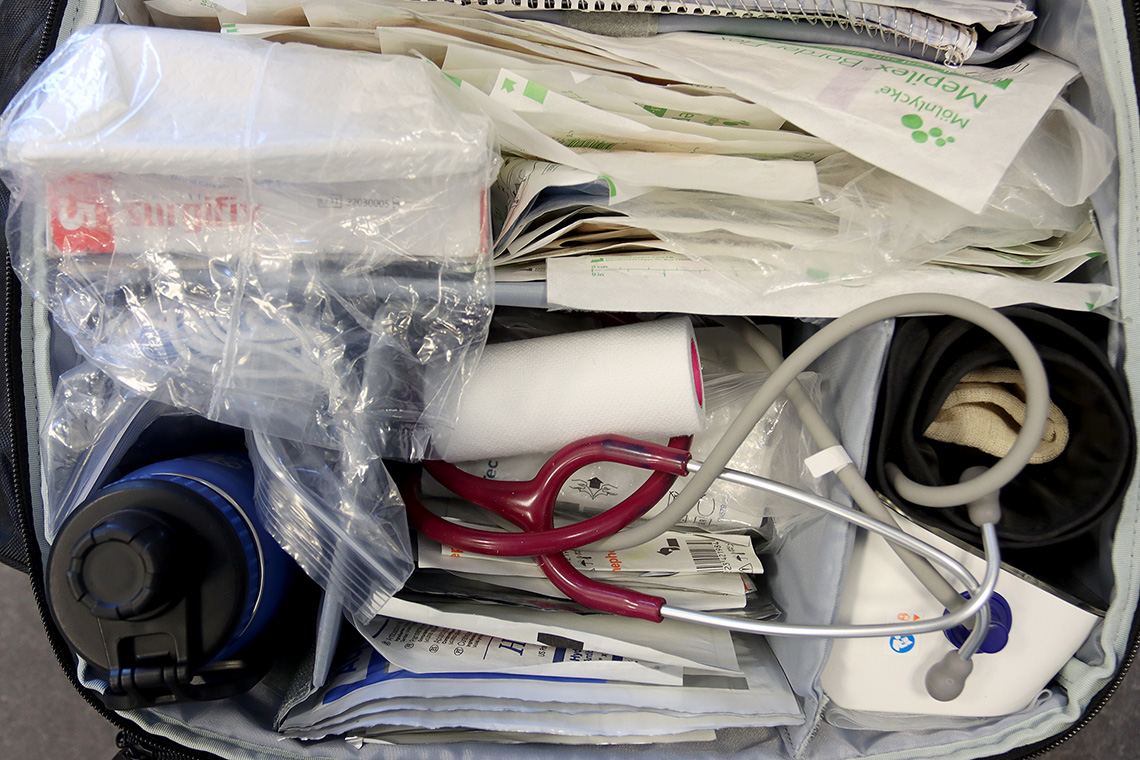
The mobile team that functions five days a week is comprised of nurses, clinicians, as well as peer support, outreach and social workers.
“We’re able to give wrap-around support,” Palomar said.
Sometimes that means distributing requisitions for blood work.
Sometimes it requires cleaning and dressing infections or providing counselling. Sometimes it’s just handing out a cup of warm coffee.
“We try not to say ‘no’ to anyone who needs help,” Palomar said.
The IHART team travels to homeless encampments, shelters and church parking lots across the northern communities of the Fraser Health district while a second team helps out in eastern communities like Abbotsford, Mission, Chilliwack, Agassiz and Hope. The service is also being extended to Surrey.
Relationship of trust
The vans follow a regular schedule so clients can anticipate their visits, Palomar said.
It also helps them build a relationship of trust, he added.
Twice a month the team offers special foot care clinics as homeless populations often have to deal with a condition called “street feet” because their shoes and socks are wet from the rain and snow.
The frontline care can help alleviate the chronic nature of health disparities the homeless population experience, said Fraser Health clinical operations director Sherif Amara.
“The vans provide an additional tool to bring care further into these remote, often secluded, settings.”
Palomar said it can also be the stepping stone to more comprehensive care and possibly even the start of a journey off the streets.
“We’re trying to bridge the gap,” he said.